When a hospital loses power, it’s not just an inconvenience. It’s a matter of life and death. Critical medical equipment relies on uninterrupted electricity to keep patients safe and hospital operations running smoothly.
Healthcare facilities require backup power systems designed to maintain essential operations during outages. This typically includes uninterruptible power supplies (UPS) for immediate protection and emergency generators capable of supporting life-saving equipment, lighting, and key building systems until normal power is restored.
The challenge for facility managers is selecting the right combination of backup power while staying fully compliant with NFPA codes. Different types of healthcare facilities and constantly evolving technology make it important to plan systems carefully to ensure safety, reliability, and regulatory compliance.
Understanding Healthcare Facility Categories and Power Requirements
Not all healthcare facilities are created equal when it comes to backup power requirements. The NFPA 99 Health Care Facilities Code uses a risk-based approach that categorizes spaces based on the potential impact of power failure on patient safety.
Category 1: Critical Care Areas
Category 1 areas are where power failure could cause major injury or death. This includes operating rooms, surgical suites, intensive care units, emergency departments, cardiac labs, and any space with life support equipment. These spaces require Type 1 Essential Electrical Systems (EES), including automatic transfer switches that start backup power within 10 seconds and generators capable of running at least 96 hours on-site fuel, with both emergency and equipment branches.
Category 2: General Patient Care
Category 2 spaces involve general patient care where power loss could cause minor injury or discomfort. Examples include patient rooms, examination areas, diagnostic imaging, labs, and pharmacies. These areas typically need Type 2 EES, though some may require Type 1 systems depending on equipment and care activities. The key differences lie in transfer times and backup capacity.
Categories 3 and 4: Support Areas
Categories 3 and 4 cover spaces with minimal risk to patient safety, such as administrative offices, storage, and corridors. Backup power is less stringent but still supports overall facility operations.
Essential NFPA Code Compliance Requirements
Healthcare facilities must follow multiple NFPA standards that work together to ensure complete electrical safety and reliability.
NFPA 99: Health Care Facilities Code
This primary standard governs healthcare electrical systems. It sets backup power levels using a risk-based method, requires EES design with automatic transfer switches, mandates a minimum 96-hour fuel supply for critical areas, and specifies monthly load testing and maintenance.
NFPA 70: National Electrical Code (NEC)
The NEC provides the foundation for all electrical installations. Article 517 addresses healthcare facilities, including grounding and bonding rules, branch circuit design for essential electrical systems, emergency lighting, and isolated power for sensitive procedures.
NFPA 110: Emergency and Standby Power Systems
This standard covers generator installation, sizing, and maintenance, fuel storage and quality checks, transfer switch performance, and acceptance testing for emergency power systems.
NFPA 101: Life Safety Code
Focused on building safety and egress, this code governs emergency lighting duration, exit sign backup power, and fire alarm system backup power.
Generator Sizing and Fuel Requirements
Properly sizing backup generators for healthcare facilities requires careful load review and future planning.
Load Calculation Methods
Essential electrical loads are divided into three branches. The Life Safety Branch includes emergency lighting, fire alarms, exit signs, and communication systems, all of which must transfer to backup power within 10 seconds. The Critical Branch covers patient care equipment such as ventilators, monitors, and surgical tools, also requiring a 10-second transfer. The Equipment Branch includes major medical devices like imaging systems, lab equipment, and HVAC systems, with transfer times up to 15 seconds.
Fuel Storage and Runtime Requirements
NFPA 110 classifies hospitals as Level 1 facilities, requiring a minimum of 96 hours of fuel for the full essential load. On-site fuel storage must include containment and monitoring, with regular fuel quality testing and treatment. Backup fuel options should be available for critical systems. Diesel generators are most common due to reliability, while natural gas systems are used where supply is stable.
Modern Backup Power Technologies
Today’s healthcare facilities have access to advanced backup power technologies that go beyond traditional diesel generators.
Uninterruptible Power Supply (UPS) Systems
UPS systems provide instant power during the short gap before generator startup. Online double-conversion UPS units protect sensitive medical equipment, while modular designs allow easy expansion and maintenance. Battery backup typically offers 15 to 30 minutes of runtime, and power conditioning safeguards against voltage fluctuations.
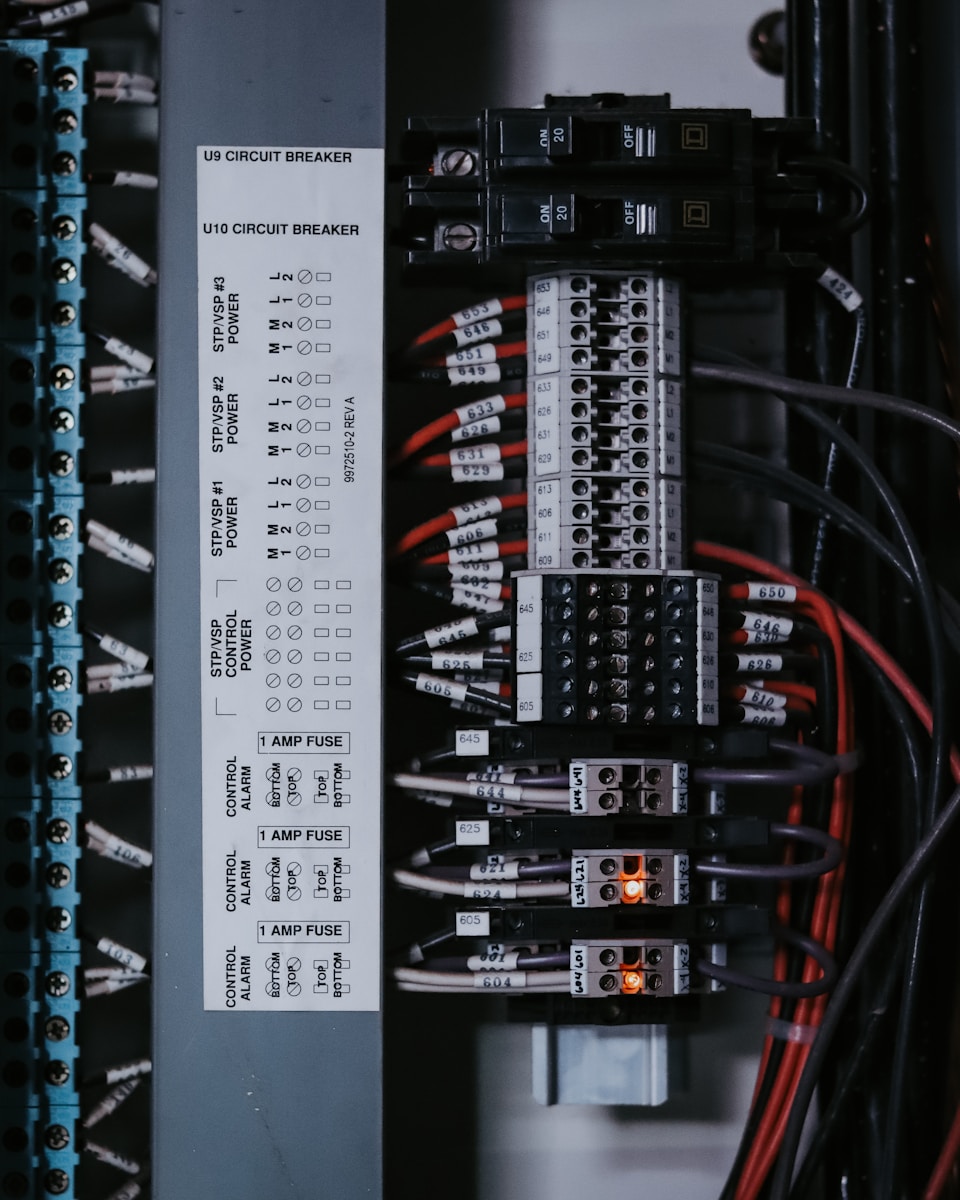
Automatic Transfer Switches (ATS)
ATS technology ensures seamless power transitions with microprocessor controls for precise monitoring and switching. Load shedding prioritizes critical systems, remote monitoring supports facility management, and bypass options allow maintenance without interrupting power.
Battery Energy Storage Systems (BESS)
BESS are emerging as complementary solutions. Lithium-ion technology delivers longer life and faster response, helps stabilize the grid during utility fluctuations, reduces demand costs through peak shaving, and can integrate with renewable energy sources.
Testing and Maintenance Requirements
Regulatory compliance extends far beyond installation. Ongoing testing and maintenance are needed for ensuring system reliability.
Monthly Testing Requirements
NFPA 110 requires monthly generator tests under load. Generators must run at a minimum of 30 percent load for at least 30 minutes. All transfer switches must be tested, fuel systems checked for level and quality, and batteries for UPS and starting systems verified.
Annual Testing Requirements
Annual tests include full-load operation at 100 percent capacity for two hours, verification of transfer switch timing, inspection of fuel system integrity, and emergency lighting duration checks.
Documentation and Record Keeping
Facilities must maintain detailed records of all tests and maintenance activities. This includes fuel usage and quality reports, system modifications and repairs, and staff training records.
Cost Considerations and ROI
Backup power systems require upfront investment, but inadequate power protection creates far greater risk for healthcare facilities.
Initial Investment Factors
Total cost depends on generator sizing, transfer switch capacity, and system complexity. Generator installations typically scale by kilowatt capacity, while transfer switches and UPS systems vary based on features, redundancy, and healthcare-grade requirements. Installation and commissioning often account for a significant portion of total project cost due to code compliance and testing.
Ongoing Operational Costs
Long-term expenses include fuel for testing and emergency use, routine maintenance contracts, and labor for required testing and documentation. Facilities may also see insurance benefits when compliant systems are in place.
Return on Investment
ROI extends beyond direct savings. Reliable backup power helps avoid downtime losses, supports patient safety compliance, reduces regulatory and insurance risk, and ensures operational continuity during utility outages.
Implementation Best Practices
Successfully implementing backup power systems requires careful planning and execution.
Design Phase Considerations
Systems should be sized for future expansion while meeting redundancy needs such as N+1 or 2N in critical areas. Designs must integrate with existing building systems, and early coordination with local code officials helps prevent compliance issues.
Installation and Commissioning
Healthcare-experienced contractors are essential to limit risk and downtime. Phased installation reduces operational disruption, while comprehensive testing confirms system performance before final acceptance. Facility staff should be trained on normal operation and emergency response.
Ongoing Management
Preventive maintenance must follow manufacturer guidance and code requirements. Performance monitoring supports reliability, emergency procedures should stay current, and technology plans should account for future upgrades or replacement cycles.
Working with Qualified Electrical Contractors
Healthcare backup power systems require specialized electrical expertise and strict code compliance. Contractors should have proven experience in healthcare facilities, strong knowledge of NFPA 99, NFPA 70, NFPA 110, and NFPA 101, and valid state and local licensing. Reviewing references from similar healthcare projects helps confirm reliability and compliance history.
At Camali Corp, our experienced team specializes in healthcare electrical systems and backup power installations. We work closely with facility managers to meet operational needs while maintaining full compliance with all applicable codes and standards.
Why This Matters for Healthcare Facilities
Healthcare facility backup power requirements are complex, but they’re essential for patient safety and compliance. By understanding the different facility categories, NFPA codes, and modern technology options, facility managers can make informed decisions about their backup power investments.
The key is working with experienced professionals who understand both the technical requirements and the operational realities of healthcare facilities. With proper planning, installation, and maintenance, your backup power system will provide the reliability and peace of mind your facility needs to focus on what matters most. Providing excellent patient care.
Remember, backup power isn’t just about meeting code requirements. It’s about ensuring your facility can continue its life-saving mission regardless of what challenges the electrical grid may face.
Need help determining the right backup power solution for your healthcare facility? Contact the experienced team at Camali Corp for a complete assessment of your facility’s requirements and a customized solution that meets all applicable codes and standards.